Organization
Ilocos Training and Regional Medical Center (ITRMC)
Best Practice Focus Area/s
Human Resource, Operations
Year Implemented
31 March 2020
This is a GBPR for COVID-19 Response entry
Summary
The vision of Ilocos Training and Regional Medical Center (ITRMC) is to provide quality multispecialty end-referral care to the people and for the hospital to level up to be the center of health capacity and response system, particularly during this pandemic. Using digital innovation to improve health access and service delivery is one important strategy to address the gaps affecting micro and macro socio-economic activities.
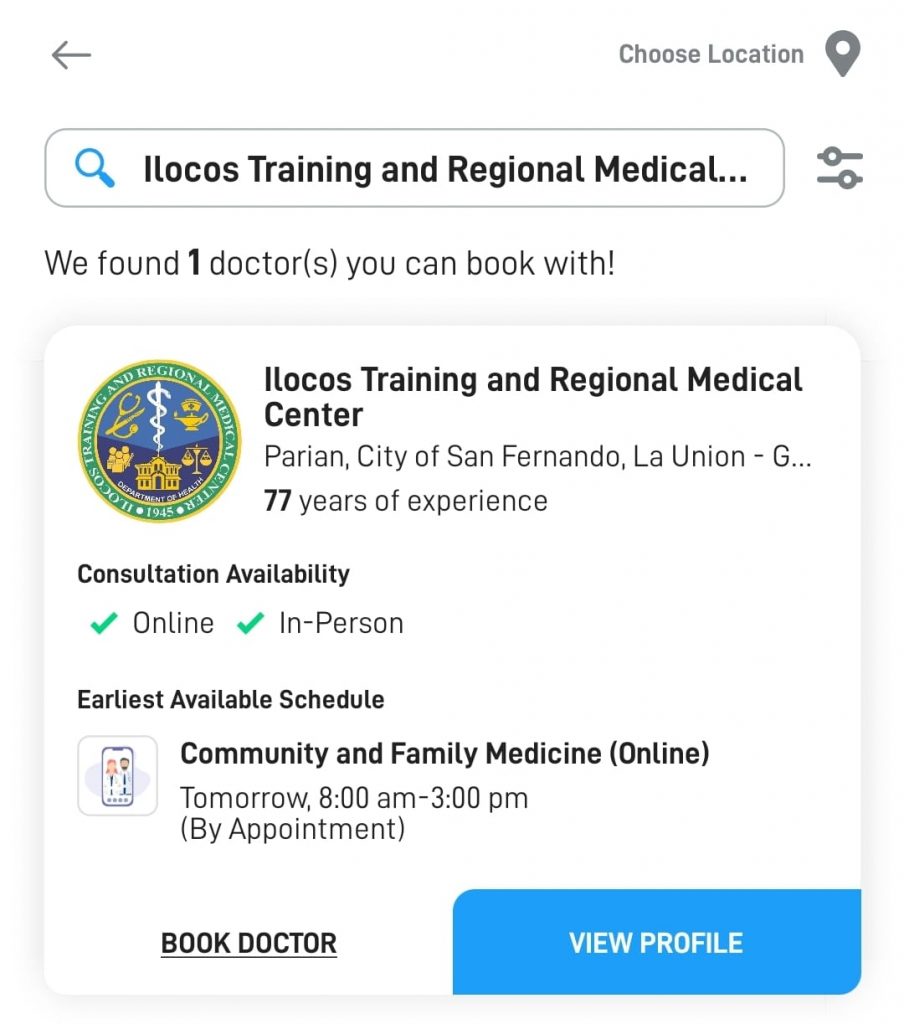
The innovation started with an online social media platform called “E-Konsulta Mo Kay Dok,” which later developed into a web application for the pre-hospital coordination Outpatient Department Appointment System. This online communication increased awareness of ITRMC as one of the few institutions that provided such services during this pandemic. It also enhances the patient experience with the hospital, provides a sense of pride, and boosts the morale of the medical team who developed the project. It has evolved to include clinical specialty and subspecialty services.
Background and Problem
Before the pandemic, the hospital caters to a daily average of five hundred (500) to six hundred (600) outpatients in a limited single-floor outpatient building that houses several specialty and subspecialty clinics. Notifiable risks include overcrowding, poor ventilation, long queues, prolonged turnaround time, inefficiency, and patient discomfort.
As the nation transitions into the “new normal,†following the Department of Health (DOH) and the directive of the Inter-Agency Task Force (IATF) on the basic minimum health standards, hospital operations must be streamlined to ensure the safety not only of the patients but also all health-care workers and the stakeholders who will visit the hospital for non-medical concerns.
Public health information is clearly and regularly given. ITRMC wants to ensure that even the most vulnerable population seeking its services will not contract the virus and other emerging infectious diseases inside hospital premises.
Solution and Impact
Last 8 June 2020, the hospital reopened its Outpatient Service, considering the five pillars of preparedness defined by the Inter-Agency Task Force: reducing vulnerability, reducing transmission, reducing contact, reducing the duration of infection, and governance and accountability in the streamlining of its operations. The initiatives include using the conceptual framework of integrated pre-hospital coordination, departmentalized and facilitated consultation, and post-hospital coordination and follow-up.
In the pre-hospital coordination, one platform used was the online consultation via e-Konsulta, which was used during the height of the Enhanced Community Quarantine (ECQ) beginning 31 March 2020. The basic principle of e-Konsulta is to provide health access using information technology via chat box through Facebook. They used it as a mechanism for surge management and to assist a patient where transportation and mobility are a concern. Another pre-hospital coordination is via call and car navigation, used by the Operation Center under Marvin Munar’s Disaster Risk Reduction Management Office.
The entire hospital’s internal business processes are currently being reviewed across all levels to address issues on quality, particularly in the following areas: safety, timely, effective, efficient, equitable, and people-centered care. All quality procedures across divisions, departments, offices, and units are in the process of review and revision with an emphasis on understanding the changes and considering the different internal and external issues brought about by the pandemic. This will be a big step in identifying mitigating actions addressing risks and using opportunities for improvement.
The post-hospital coordination with all health care facilities, including institutions involved in public health, will be strengthened by establishing a unified database of information technology, capacity-building activities, and financial integration embedded in the Universal Health Care Act. The impact is the improvement in hospital operations, thus ensuring delivery of quality care along with the following major areas: safety, effectiveness, efficiency, equitability, timeliness, and people-centeredness.
Milestones/Next Steps
Before the official opening of the OPD, a two (2)-day dry run was held to observe for process flow, compliance with basic health standards, avoiding overcrowding, turnaround time, and compliance with infection control and triage protocols. The dry run result and the effect after less than a month of implementation will be reported under the performance measures and impact.
Congruent with this, the Operation Center has launched a data-collection system on pre-hospital coordination relative to the operation of the Health Care Provider Network with the Local Government of La Union. They will use the information captured as a way forward to improve pre-hospital coordination not only among healthcare facilities but also with the community at large.
In the same way, the data encoding system was reviewed and revised to strengthen intrahospital or interdepartmental referral and communication to improve the Outpatient consultation for follow-up care after hospital discharge.
The ITRMC is planning to enhance further and improve the technology to include a unified database sharing of electronic medical records with their existing partners in the province-wide Health Care Provider Network, including but not limited to Provincial and District Hospitals and Rural Health Units. This will be an excellent opportunity to further gather health information for translational research to improve healthcare service delivery and partnership.
